A Trainer's Guide to Thoracic Outlet Syndrome
Thoracic Outlet Syndrome(TOS) is a pretty unnerving condition(you'll get that joke later) that festers our community. It can be the result of trauma, poor posture, overuse or even deformity and should only be diagnosed by a qualified professional. With that being said, it's not uncommon for a trainer or coach to end up with clients who have TOS. In fact, in some sport, namely overhead ones, you will most likely run across several cases of it. It's always best to refer out when you see chronic signs of TOS, but there will be many times when the client comes back from their rehab after the symptoms may have subsided, but the underlying causes are still present. It's for that reason that you should have an understanding of what is at play to give them the best results possible and try to restore function to the area within your professional means.
Overview
Thoracic Outlet Syndrome is defined as a condition that causes pain in the neck/shoulder and usually consist of tingling or numbness within the hand/fingers and a weak grip. As you can see the classic definition doesn't give you a lot to go off of and as I said earlier, it can be due to trauma, posture, over-use or even deformity. For the purpose of this article, we'll only be looking at that within our scope: posture/over-use and their overlap with muscle function.
The symptoms of TOS are caused by the compression of the neurovascular bundle in the thoracic outlet(area between the first rib and collarbone). This bundle consists of the subclavian vessels and the brachial plexus, which explains the tingling and numbness in the hand. Now when examining the picture below, you can see how this bundle passes through the scalenes and under the pec minor. These are the structures that are often responsible for compressing the bundle.
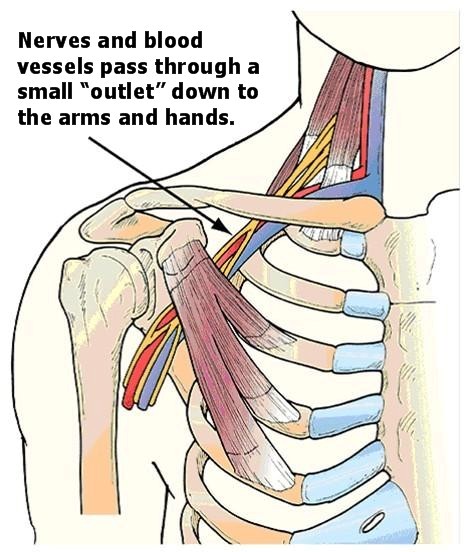
Two less thought of culprits not shown in the picture above are the subscapularis and coracobrachialis. Both of these tissues can aid in compressing the neurovascular bundle and should be especially examined in overhead athletes showing signs of TOS.

Assessment
Any of these four muscles play a major role in dealing with TOS. Often times if the client is coming from a rehab professional, they will already know where the dysfunction lies and can point you right to the issue. Other times it may not be so obvious and you may have do some snooping around to figure out what fibers seem to be the culprit. This is where movement screens or manual muscle testing can make a world of difference. Palpating tone can also be extremely helpful if that is in your scope of practice(careful trainers). Adison's and Reverse Adison's Tests are two orthopedic tests that you can use to determine if the anterior or medial scalenes are compressing the bundle and Wright's Test to see if it's an issue with the shoulder musculature.
http://www.youtube.com/watch?v=0FVvOAndbwk
With these assessment tools in your toolbox, it's very important that you remember this: YOU CANNOT DIAGNOSE. That is a clinician's job. Your job is to get them moving and feeling better. Leave the pathologies to the docs and always refer out when the client is in pain or if it persists. But, just as a sit and reach tells about tight hamstrings (Well, kinda..), we can use the information from these tests to help determine what muscles may be shortened and limiting their movements.
Once you feel that you have determined which fibers are the culprits, it's important that you do not go guns blazing and smash the crap out of the pec minor. Again, your job is to make them move and feel better. Muscles get tight for a reason and that reason needs to be addressed. Will stretching those fibers help to decrease the compression? Yes, but unless the reason is addressed, they will tighten right back up before the end of your session. Often times there is a muscle imbalance, movement dysfunction or even fascial adhesion that may be causing that pec minor to increase in tone, shorten up and compress the neurovascular bundle. So once the compressing fiber has been found, put that information together with their subjective movements and work your way to victory through corrective strategy. Just remember that the area of pain is seldom the cause of the pain.
The Scalenes
Increased tone and shortness of the anterior or middle scalene can point to a number of things, especially considering they have multiple functions. Mainly keep in mind that they help to elevate the first rib and laterally flex the neck to the ipsilateral side.
Since the scalenes help to elevate the ribs, this means that they are also accessory breathing muscles. Just another reason why you should always assess breathing. If the client seems to be a neck breather, priority number one should be to restore their diaphragmatic breath. It's no wonder that those muscles are getting tight if they're doing 10,000 reps a day to make sure you stay alive. Now because breathing is so closely tied to the limbic system and sympathetic tone can have a HUGE impact on the quality of breath they take, the root cause of dysfunction may be multifaceted. It may take more work than the usual, "just breath through your belly" drill. Relaxation techniques may be a necessary start and utilizing methods from PRI, DNS or Restorative Breathing can do wonders.
As cervical lateral flexors, the scalenes can also be primo compensators for dysfunctional cervical rotation. If you notice that they tend to turn their head as if they're talking on the phone, that's a pretty likely sign that the rotation needs to be cleaned up. This can get pretty complicated and is good for you to know about when considering exercises for their training. A dysfunction in cervical rotation means there will likely be a dysfunction in lumbar and/or thoracic rotation and you will need to adjust accordingly. Because of the intricacy of the neck, this is a situation in which you should leave all the direct work to the rehab professionals unless you've had special training. Otherwise, focus on creating rotational stability in other segments through oblique and multifidi-based drills. Here are two of my favorite drills:
http://www.youtube.com/watch?v=q1l7Rf1dNPc
http://www.youtube.com/watch?v=RHsWxdn-kGE
The Pec Minor
The dreaded pec minor. Every trainer has clients with pec minor issues and if they say they don't, they aren't looking closely enough. The pec minor is the main anterior stabilizer of the scapula and assists in downward rotation, depression and protraction of the shoulder blade. It also is an accessory breathing muscle so as stated with the scalene, breathing should be closely examined.
As a scapular stabilizer, pec minor dominance is pretty well known and written about, so I'm not going to spend time discussing it's mechanics versus the traps or lats(if you are interested in learning about that, I recommend checking out some of Eric Cressey's articles). But, I would like to point out how far the pec minor's function can reach.
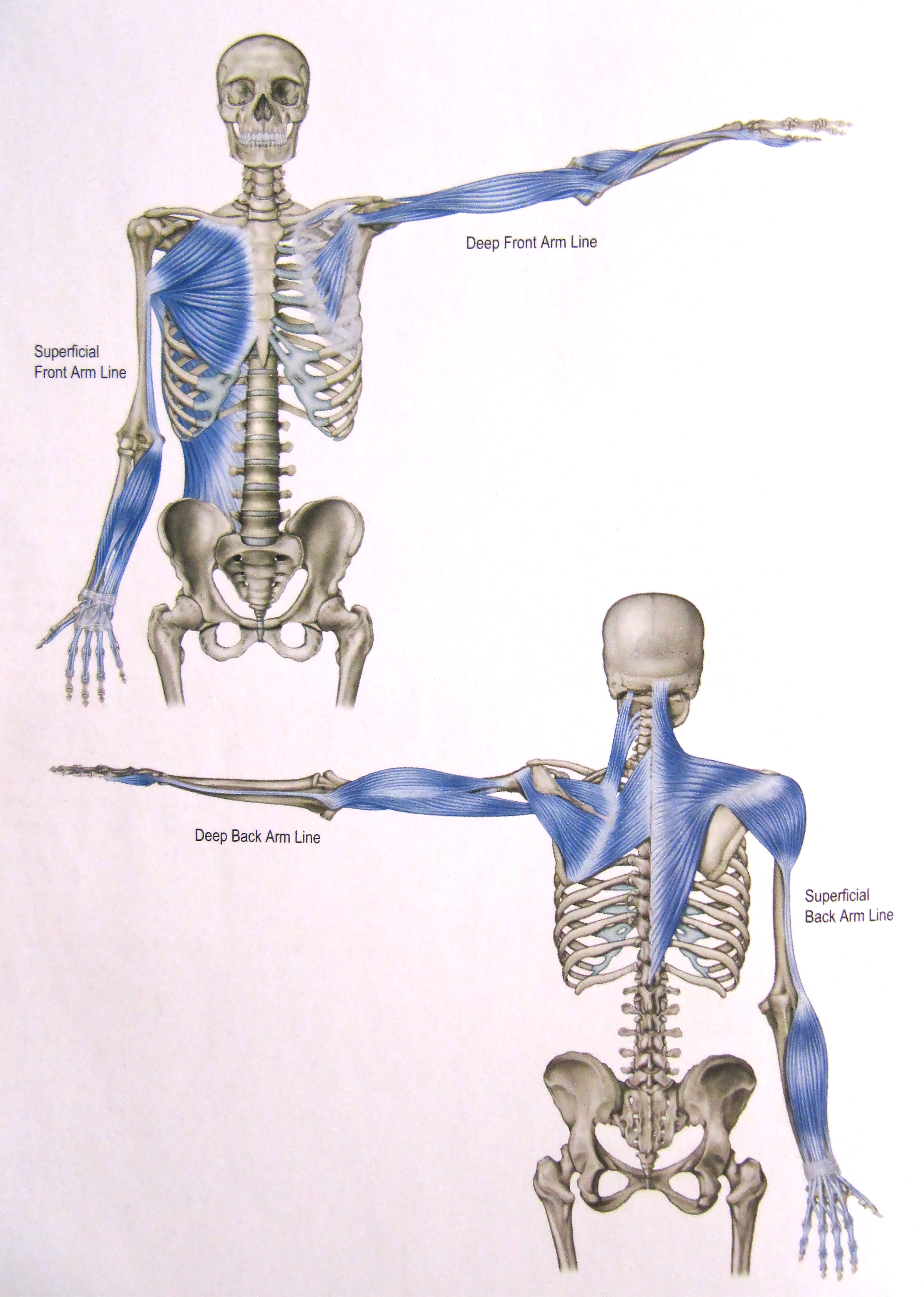
The pec minor is part of Thomas Myers' Deep Front Arm Line. The Deep Front Arm Line is the layer of fascia enticing the muscles shown below. Because of this, these muscles share a lot of neurological connections and will contract to create tension through the line when there is instability. You'll notice that the connection goes all the way down to the thumb. This means that grip dysfunction can easily place more load on the pec minor and add to it's tonicity. This is another reason why being observant to how your client moves is important. If you notice more protraction/downward rotation as they grip weights, then there is likely a dysfunction in their Deep Front Arm Line. This will require special grip work along with a nice, cozy lacrosse ball to the pec minor.
The Subscapularis
The subscapularis is going to be a critical point to examine in OH athletes. Of course it should be assessed in any client with a history of TOS, the violent movements of throwing puts it at a higher chance of dysfunction than other fibers amongst many overhead athletes. Not only has it been noted to be the most important player in stabilizing the humeral head within the glenoid capsule, researchers have found that it contributes to about 53% of cuff movement through the action of a throw. It contracts especially hard during the acceleration phase of delivery along with with the serratus anterior, pectoralis major and latismus dorsi to concentrically internally rotate the humerus.
Knowing these relationships can be a game changer when evaluating shoulder mechanics and their relation to TOS. If the other rotator cuff muscles are weak or dysfunctional, this will put more of a strain on the subscapuaris which is already doing a majority of the stabilization of the humeral head. This goes the same for the synergists that help to internally rotate the humerus through the acceleration phase. If one or more of these muscles show weakness or dysfunction (cough cough winged scapula cough cough) then the subscapularis will also try to take up the slack and become very taught.
It's also worth mentioning that fibers of the subscap will often form adhesions. This can be for a number of reasons, but in our overhead populations, can usually be attributed to overuse. Palpation will usually help to confirm this(if you can) and often times will be found where the subscapularis runs into the serratus anterior. Friction and other release techniques have been found to be very effective in this situation, but again, only do what is in your scope.
The Coracobrachialis
The coracobrachialis is a hugely overlooked muscle within regards to shoulder function in my opinion. It assists with shoulder flexion and horizontal adduction as well as a little bit of internal rotation. For these reason, it can become taught for many different dysfunctions within the shoulder girdle. Just like every other muscle that I've mentioned thus far, there can be a large number of relationships to look for. It's been noted that the coracobrachialis is an especially large player in stabilizing the glenohumeral joint when at rest in a relaxed, standing posture. As such, working on general shoulder mechanics and posture can be very helpful.
In Closing
As you can guess, there can be many different relationships that could cause the aforementioned fibers to compress the neurovascular bundle. The examples that I listed are just that, examples. It's up to you to use your tools as a trainer to figure out what movement dysfunction is causing the shortening of the fibers. Working to loosen up the fibers will help an issue, but working to restore function will help fix an issue.
The main point of this article is to always look at the bigger picture. As trainers, we usually see clients more often than traditional rehab professionals and as such, we should be working on total body function, especially as it relates to our client's goals and problem areas. Doing so can expedite progress of any rehab program the client may be in or can even ensure that their pain stays away. Physical therapists and chiropractors are often times restricted by insurance and time as to how much they can truly help with an individual's movements. Their hands are usually tied to getting the individual out of pain and rarely do they get a chance to completely eradicate the root cause for the pain. This is where a good trainer should come in and assist to correct movement and strength to prevent a relapse of symptoms. Working hand in hand with rehab professionals and referring out when needed is extremely important. Sticking to your scope of practice not only protects you, but also ensures your client gets what they need from you. As you can see from this article, there is still a lot you can do.
